The Insulin Factor: Can’t Lose Weight? Can’t Concentrate? Can’t Resist Sugar? Could Syndrome X Be Your Problem?
Whilst your total score is perhaps the most important indicator of overall risk for Insulin Resistance, the individual parts also have relevance. Both are categorized according to risk in the table below.
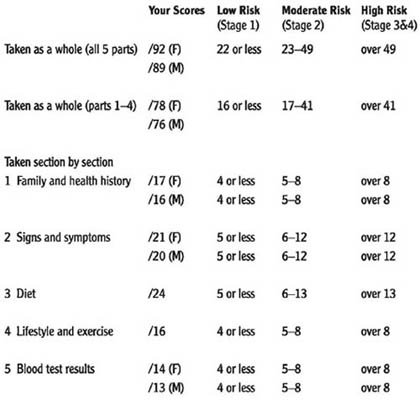
The Insulin Resistance questionnaire indicates the degree of Insulin Resistance you may have. The following text clarifies your risk of Insulin Resistance, and will help you plan your dietary and lifestyle changes.
1 Family and Health History: As only two elements in this section can change (weight and age), this is a relatively fixed score. This sets the scene for your risk, but does not determine it.
2 Signs and Symptoms: If you scored highly on this part of the questionnaire, together with a moderate risk total score or more, it suggests that you could be at a moderately advanced stage of Insulin Resistance, particularly if you are overweight. You need to follow all parts of the Insulin Factor Plan.
If you score highly on this section but only score a low risk on all other parts of the questionnaire, then consider taking the Adrenal Stress Profile saliva test and study chapter 9 on stress. You will also need to follow the dietary plan in chapter 13, and the Adrenal Support Supplement Programme.
3 Dietary Factors: If you scored highly on this part but not on the others, this puts you at risk of being in the early stages of Insulin Resistance, and increases your risk of developing it in due course. Eating refined carbohydrates represents the single biggest risk factor for developing Insulin Resistance. This risk is more pronounced if you score highly in part 4, Lifestyle and Exercise. You need to concentrate on the dietary plan in chapter 13, and follow the Insulin Resistance Supplement Plan One.
4 Lifestyle and Exercise: If you score highly in this section only then is there a need to start becoming more physically active. Even if you are not overweight you could well be in the early stages of Insulin Resistance. Inactivity is a profoundly important risk factor for Insulin Resistance, especially if you’ve scored highly in part 3 of the questionnaire, Dietary Factors. You need to read chapter 10 and find out the most suitable exercise for you.
5 Blood Test Results: These give ‘hard’ evidence of your current degree of Insulin Resistance, which is examined in more detail here. It is unlikely that a high score in this part would not be matched by high scores in other parts of the questionnaire. Don’t worry if your test results score highly: it doesn’t mean you can’t change them, far from it. In fact, the blood tests are an excellent way to monitor your improvements when you implement the Insulin Factor Plan.
Improving your situation
Your total questionnaire score, for either four or five parts, represents your baseline score, which will improve when you begin to implement the Insulin Factor Plan. Please redo parts 2 to 4 or 2 to 5 inclusive (not part 1, unless you have lost weight and are a year older) one month after you begin any changes in diet, nutrition and exercise to see the reduction in your scores. This is a good way of monitoring how you are doing, and will hopefully encourage you to keep going. If your score does not go down at all, please review chapter 12, which provides you with the model of how to reverse Insulin Resistance, and double check that you have gone through the action steps and check lists. If, within another month, there is still no change, it would be best to go and see a qualified nutritionist (see Resources).
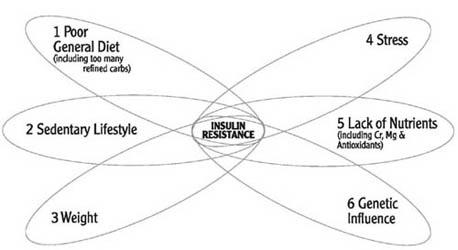
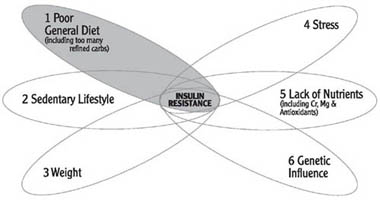
There are many other questionnaires in this book but the Insulin Resistance questionnaire is the most important. Keeping your results of the questionnaires in mind, let’s now take a look at the six major causes of Insulin Resistance and how your questionnaire results tie in with them.
The six major causes of Insulin Resistance
There are six major causes of Insulin Resistance and your results from the questionnaires will show you how much of a contributor each one is to you.
1 General diet: eating too many refined carbohydrates and over-processed foods (this includes low nutrient levels and an imbalance in dietary fats – see chapters 5–8)
Measured by the Diet Questionnaire
2 Sedentary lifestyle: lack of physical activity and exercise, and lack of muscle (see chapter 10)
Measured by Exercise and Lifestyle Questionnaire
3 Weight: being overweight and/or having an elevated BMI (see this chapter)
Measured by BMI calculation, observation and body composition measurements
4 Stress: abnormal stress hormones (cortisol and DHEA) have a negative effect on Insulin Resistance (see chapter 9)
Measured by Stress Questionnaire and adrenal hormone saliva test
5 Lack of nutrients: chromium, magnesium, essential fats, other nutrients (trace minerals, minerals, vitamins) including antioxidants (see chapters 6, 7 and 8)
Measured by Diet and Signs and Symptoms Questionnaires and blood tests
6 Genetic influence: a family history of diabetes, heart disease and obesity and being of South Asian, African, Polynesian or Mexican origin (see chapter 11)
Measured by Family and Health History Questionnaire
The Insulin Connection
Age and insulin
Whatever your ethnic origin, your risk of Insulin Resistance increases as you get older. If you remain active, take gentle exercise to reduce loss of muscle mass, reduce the amount of calories you eat but increase the quality of your nutrient intake (as we age we become less efficient at digesting food), your age will not work against you and you will also find that you age more slowly.
However, it is also true that Insulin Resistance is becoming increasingly common in younger and younger people and a person’s chronological age is a less obvious risk factor than it once was. In actual fact, people who develop Insulin Resistance as early as the late teens and early twenties have a prematurely aged metabolism – i.e. they have the metabolism you’d expect to see in someone at least twice their age. Don’t worry if this sounds like you. Not only will the Insulin Factor Plan put your insulin and glucose levels back on track but it will also help you take years off your body’s biological age – the best kind of side-effect!
See Resources for help interpreting your Insulin Resistance Blood Test.
If you have done a blood test and know what degree of Insulin Resistance you have, turn to the Resources. However, without a blood test you can still get a good idea about what degree of Insulin Resistance you have, and take the appropriate action as outlined below. Your questionnaire scores will reflect a low, moderate or high risk of Insulin Resistance, which correlate with the different stages of Insulin Resistance that would be determined by the blood test.
Low Risk – Stage 1
You are insulin sensitive, and insulin levels fluctuate depending on food and drink intake, but you have normal fasting insulin and glucose levels. This does not mean you are free of symptoms, since you can put on weight if you eat too much, but this is not a dramatic or rapid process. You can also get symptoms of low blood sugar after eating a sugary meal like a big baked potato, because your insulin works well and is stimulated in large amounts by the high-sugar potato and consequently stores glucose into liver, muscle and fat cells rapidly, resulting in ‘post-prandial hypoglycaemia’. At this stage your blood test results would all be normal.
Action: Follow the Insulin Factor Diet Plan and Insulin Resistance Supplement Plan One
Moderate Risk – Stage 2
Your fasting insulin is still normal, as is your glucose. However, you can gain body fat more easily in this stage, and your fasting triglycerides (blood fats) would be elevated and the good cholesterol (HDL) low.
Action: Follow the Insulin Factor Diet Plan and Insulin Resistance Supplement Plan Two
High Risk – Stage 3
Your fasting insulin is elevated, as it is after eating, the triglycerides (blood fats) are high too and the HDL is low, and, generally, you are overweight, especially around your middle.
Action: Follow the Insulin Factor Diet Plan and Insulin Resistance Supplement Plan Three
High Risk-Stage 4
Your scenario is the same as for stage 3 above, except that your fasting blood glucose is a little too high.
Action: Follow the Insulin Factor Diet Plan and Insulin Resistance Supplement Plan Three
Stage 5
At this stage you would technically be diabetic because your blood glucose would be too high.
Action: Follow the Insulin Factor Diet Plan and follow doctor’s drug prescription. Supplements may be appropriate but should be recommended by a qualified nutritionist working with your doctor.
So, now you know your risk of Insulin Resistance. However, before you get going with the Insulin Factor Plan you need to take a closer look at the diet and lifestyle influences that will really make a difference to the speed at which you reverse Insulin Resistance. These are the two main areas of change that you will form part of your Insulin Factor Plan and getting to grips with them will make it much easier for you to succeed.
Summary of key points







Digestive problems are a hidden cause of Insulin Resistance. This is mainly because as much as 70 per cent of the body’s immune system is located within the gut, and if your gut immunity is taxed the gut is flooded with cytokines – if you remember these are immune messengers – and in large quantities these blunt receptors for insulin in your body. This means insulin becomes less effective at storing glucose away so the body produces more insulin to compensate. For example, this is why, if you have a food intolerance, you can have difficulty in losing weight: your immune system is battling with a perceived threat and, in producing cytokines to fight it, interrupts the usual efficient function of insulin.
It’s not just food intolerances that cause an immune reaction in the gut: yeasts such as candida albicans, unfriendly bacteria, parasites and maldigestion trigger cytokine activity as well. Poor diet is a major culprit since not only does it not provide adequate nutrients for optimal immune function but it creates an environment within the gut that favours and feeds unwanted bugs.
The other thing that causes or exacerbates the likelihood of both gut problems is stress. Stress directly weakens immunity within the gut, thereby leading to an inability to distinguish friend from foe (i.e. overreacting to an everyday food) and prevent the colonization of unwanted bugs.
Digestive problems are extremely common as the typical Western diet is high in refined foods and we lead high-stress lifestyles.

Gut Health Questionnaire
Answer ‘yes’ or ‘no’ to the following questions. Each ‘yes’ answer is awarded a single point. Your total score will help you determine the likelihood of your digestive system contributing to Insulin Resistance.
Do you regularly (every few days) have:
1 Indigestion or heartburn?
2 Bloating after meals?
3 Nausea?
4 Excess flatulence?
5 Abdominal pain?
6 Cramps?
7 Irregular bowels?
8 Diarrhoea?
9 Constipation (less than one motion per day)?
10 Haemorrhoids (piles)?
11 Known or suspected food intolerances?
12 Antibiotics?
13 Anti-pain medications (e.g. aspirin or ibuprofen)?
14 Yeast or candida overgrowth?
15 Parasite or gut bacterial infections?
16 Food poisoning?
17 More than 14 units of alcohol per week?
Score out of 17 =
If you have any one of these regularly then your digestive health needs attention. If you’ve scored more than 5 then it almost certainly means it is compromising your Insulin Resistance, and warrants immediate action. If you have a pattern of any of these symptoms after eating specific foods then this suggests you have a food intolerance and this could be affecting your insulin sensitivity. It would be worth your while eliminating the suspected culprit food for a trial period of four weeks to see if your symptoms improve.
To address any digestive problems start the Insulin Factor Diet Plan and the Gut Supplement Plan rather than the Insulin Resistance Supplement Plan. It may take a number of weeks to reduce your questionnaire score, and only when you have reduced the score to 4 or less, and the symptoms are less regular, should you start following any of the Insulin Resistance Supplement Plans.
Summary of key points







The Insulin Connection
Mixed messages
With all this discussion about refined sugars and carbohydrates you may be wondering if you should still be eating them, particularly as we are bombarded on a daily basis with conflicting opinions and information on what we should and should not be eating. First we are told that ‘fat is bad’, then it’s carbohydrates. What are we to do – not eat either? And how can we do that when we’ve been told that too much protein isn’t good for us either? It’s hardly surprising there are a lot of confused people.
What the headlines – and often the articles themselves – fail to explain is that there are good and bad fats, good and bad carbs, and good and bad proteins, all of which should ideally be eaten in balance with each other for optimum health. They also make an assumption that we are all the same, which is evidently not the case as each of us requires a different balance of nutrients to achieve good health. Take twins for example: they can have up to a twenty-fold difference in needs for some nutrients.1 Imagine how different it could be between people who are not related!
To help you start to get to grips with some useful nutritional facts, this chapter looks at carbohydrates and fibre, the Glycemic Index, and then proteins. Lastly you’ll find out what proportions of carbs and protein you should eat to reverse Insulin Resistance.
There are two questionnaires to help you figure out what kind of carbs and proteins you are eating. The carbohydrate questionnaire is the first.
The Carbohydrate Questionnaire
Scoring the questionnaire
Each ‘yes’ answer scores 1 point.
Do you regularly:
1 Eat sugar or hidden sugars in food or drink?
2 Eat packet foods such as breakfast cereals?
3 Eat white flour products (e.g. bread, pasta, biscuits, cakes) and/or white rice more than 5 times a week?
4 Crave sweet foods?
5 Smoke cigarettes?
6 Drink more than 2 glasses of wine or beer a night?
7 Drink more than 3 cups of tea a day?
8 Drink more than 2 cups of coffee a day?
9 Drink fizzy drinks on most days?
10 Feel dizzy or irritable after 3 hours without food?
11 Get nauseous if you go without food, especially in the morning?
12 Get the shakes if you go without food for too long?
13 Get headaches if you miss a meal?
14 Need to eat frequent meals?
15 Pee a lot during the day and night?
16 Have excessive thirst?
17 Have cold hands and feet?
18 Get tired?
19 Get anxious and stressed?
20 Work harder than most people?
21 Wake up in the night feeling hungry?
22 Are you addicted to carbohydrates/sweet foods?
Total Score = /22
Interpreting the questionnaire
A high score in this questionnaire means you consume too many refined carbohydrates and this contributes to and increases your risk of Insulin Resistance. As you make changes to your diet, you should see your score reduce. Reading this chapter will help you understand why the wrong carbs are the major cause of Insulin Resistance.
0–5 Excellent! Keep your carb balance at this level. If you scored 5 or just under, see if you can score even lower by following the Insulin Factor Plan. 6–10 This suggests you have a blood sugar problem, which is caused by your diet. To resolve this as swiftly as possible you should to follow the Insulin Factor Diet Plan and the Insulin Resistance Supplement Plan One. 11–15 Too much! This strongly indicates a blood sugar and insulin problem, and that your diet is the major culprit. You need to follow the Insulin Factor Diet Plan and the Insulin Resistance Supplement Plan that your Insulin Resistance Questionnaire indicated in chapter 3. You should also redo this questionnaire in four weeks’ time to check your progress. 16+ Much too much! There’s no doubt that your diet is a significant causative factor in your Insulin Resistance. You may benefit from doing the Insulin Resistance Blood Test. You need to follow the Insulin Factor Diet Plan and the Insulin Resistance Supplement Plan that your Insulin Resistance Questionnaire indicated in chapter 3. You also need to consider testing and balancing your adrenal hormones (see chapter 9). Use the questionnaires to monitor your progress. After four or five weeks, if there is no marked improvement despite changing your diet you should see a qualified nutritionist (see Resources).Carbohydrate groups
Most foods actually contain a mixture of carbohydrates, proteins and fats; it’s rare for any food to contain only one of these macro-nutrients. Some foods are dominant in carbohydrates, some dominant in protein and some in fat. Carbohydrate dominant foods consist of cereals, grains, starchy vegetables and fruits. Legumes (beans and pulses) also contain predominantly carbohydrates even though they are often referred to as a protein food. Meats, fish, poultry and eggs have little or no carbohydrate content, whilst dairy products can contain the carbohydrate lactose (milk contains more than hard cheese) and soy products can contain carbohydrates, depending on the type (e.g. tofu, soy milk, tempeh). Nuts and seeds have little or no carbohydrate (the cashew nut contains the most, with 18 per cent of its weight as carbs). Non-starchy vegetables also contain some carbohydrates but in much smaller amounts than their starchy counterparts.
The most simple carbohydrates are known as simple sugars or monosaccharides. These are the fundamental building blocks of carbohydrates, just as the amino acid is the building block for proteins. When you eat a simple sugar or refined carbohydrate it requires little or no digestion and is absorbed quickly into the bloodstream. This elicits a rapid and excessive insulin response, and it is for this reason that refined carbs are so bad for you. The human body is not designed to handle REGULAR intake of refined carbohydrates with impunity.